Components Of Blood and Their Functions
The components of blood include plasma, platelets, and red and white blood cells that circulate through the body. Blood supplies essential for all living organisms
RENAL PHYSIOLOGY AND BLOOD
BLOOD AND IT'S COMPONENTS
Blood has two primary components:
1. Blood Plasma: A watery liquid extracellular matrix containing dissolved substances.
2. Formed Elements: Cells and cell fragments.
Centrifuged Blood Composition
- Blood composition: 45% formed elements, 55% plasma.
- Formed elements: Over 99% are red blood cells (RBCs). White blood cells (WBCs) and platelets make up less than 1%.
- Centrifugation: Cells settle at the bottom, plasma forms the top layer. A thin buffy coat layer of WBCs and platelets forms between RBCs and plasma.
Blood Plasma
- Composition:
91.5% water, 8.5% solutes.
- Proteins:
7% of plasma by weight. Plasma proteins maintain blood osmotic pressure.
- Synthesized by Hepatocytes:
Albumins (54%), Globulins (38%), Fibrinogen (7%).
- Gamma Globulins:
Produced by certain blood cells during immune responses. Known as antibodies or immunoglobulins, they target and neutralize antigens like bacteria and viruses.
- Other Solutes: Electrolytes, nutrients, regulatory substances (enzymes, hormones), gases, and waste products (urea, uric acid, creatinine, ammonia, bilirubin).
Formed Elements
Three main components:
1. Red Blood Cells (RBCs): Whole cells responsible for oxygen transport.
2. White Blood Cells (WBCs): Whole cells with various immune functions.
- Granular Leukocytes (visible granules under a light microscope after staining):
1. Neutrophils
2. Eosinophils
3. Basophils
- Agranular Leukocytes (no visible granules under a light microscope after staining):
1. T and B lymphocytes and natural killer (NK) cells
2. Monocytes
3. Platelets: Cell fragments involved in blood clotting.
Hematocrit
- Definition: The percentage of blood volume occupied by RBCs.
- Normal Ranges:
- Adult females: 38–46% (average 42)
- Adult males: 40–54% (average 47)
- Factors Influencing Hematocrit:
- Testosterone: Stimulates erythropoietin (EPO) production, increasing RBC production.
- Menstruation: Can lower hematocrit in females due to blood loss.
- Conditions:
- Anemia: Lower-than-normal RBC count, indicated by a significant drop in hematocrit.
- Polycythemia: Abnormally high RBC percentage (hematocrit 65% or higher). Increases blood viscosity, leading to higher blood pressure and stroke risk. Causes include abnormal RBC production, tissue hypoxia, dehydration, and EPO use by athletes.
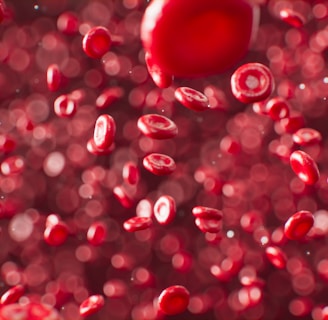
Red Blood Cells (RBCs)
Overview and Structure of RBCs
Red blood cells (RBCs), or erythrocytes, contain hemoglobin, a protein that transports oxygen and gives blood its red color.
A healthy adult male has about 5.4 million RBCs per microliter (µL) of blood, while a healthy adult female has about 4.8 million.
New RBCs are produced at a rate of 2 million per second to balance the destruction of old RBCs.
RBC Anatomy
RBCs are biconcave discs, 7–8 µm in diameter, which allows flexibility and deformation through narrow capillaries.
Their plasma membrane is strong and flexible. They lack a nucleus and organelles, enabling space for hemoglobin, which makes up 33% of the cell's weight.
RBC Physiology
- The absence of a nucleus in mature RBCs maximizes space for hemoglobin, enabling efficient oxygen transport.
RBCs generate ATP anaerobically, ensuring they do not consume the oxygen they carry.
Each RBC contains about 280 million hemoglobin molecules. Hemoglobin consists of globin (four polypeptide chains) and heme (a ring-like nonprotein pigment with an iron ion at its center).
Hemoglobin binds up to four oxygen molecules, releasing them in tissues. It also transports 23% of carbon dioxide, releasing it in the lungs.
Hemoglobin binds nitric oxide (NO), which causes vasodilation and improves blood flow.
RBC Lifecycle and Production of RBCs
RBC Lifecycle
- Lifespan and Wear: Red blood cells (RBCs) have a lifespan of about 120 days. They experience significant wear and tear as they travel through the circulatory system, especially through narrow capillaries.
- Aging and Fragility: As RBCs age, their plasma membranes become more fragile and are more likely to rupture. This is particularly true when they pass through the narrow channels of the spleen.
- Destruction and Recycling:
1. Phagocytosis: Ruptured and worn-out RBCs are phagocytized by macrophages in the spleen, liver, or red bone marrow.
2. Hemoglobin Breakdown: The hemoglobin molecule is split into its globin and heme components.
3. Globin Reuse: Globin is broken down into amino acids, which can be reused for protein synthesis.
4. Iron Transport: Iron is removed from the heme group in the form of Fe3+ and binds to the plasma protein transferrin, which transports it in the bloodstream.
5. Iron Storage: Fe3+ detaches from transferrin and binds to ferritin, an iron-storage protein, in muscle fibers, liver cells, and macrophages.
6. Recycling of Iron: When needed, Fe3+ reattaches to transferrin and is transported to red bone marrow, where it is used in hemoglobin synthesis.
7. Heme Conversion: The non-iron portion of heme is converted to biliverdin, a green pigment, and then to bilirubin, a yellow-orange pigment.
8. Bilirubin Transport: Bilirubin is transported to the liver and released into bile, which eventually reaches the intestines.
9. Intestinal Conversion: In the large intestine, bacteria convert bilirubin to urobilinogen. Some urobilinogen is reabsorbed and excreted in urine as urobilin, while most is converted to stercobilin and excreted in feces, giving feces its brown color.
Production of RBCs (Erythropoiesis)
- Initiation in Bone Marrow:
Erythropoiesis starts in the red bone marrow with precursor cells known as proerythroblasts.
- Cell Development:
Proerythroblasts undergo several divisions, producing cells that begin to synthesize hemoglobin.
- Nucleus Ejection:
Near the end of their development, these cells eject their nucleus and become reticulocytes. This ejection creates the distinctive biconcave shape of RBCs.
- Reticulocyte Maturation:
Reticulocytes contain some residual organelles and pass from the bone marrow into the bloodstream by squeezing through endothelial cells of capillaries. They mature into fully functional RBCs within 1-2 days.
- Regulation by Oxygen Levels:
- Negative Feedback System: Erythropoiesis is regulated to maintain the balance between RBC production and destruction. If the blood's oxygen-carrying capacity drops, a feedback mechanism increases RBC production.
- Hypoxia Response: Hypoxia, or low oxygen levels, stimulates the kidneys to release erythropoietin (EPO). EPO accelerates the maturation of proerythroblasts into reticulocytes, increasing the number of RBCs and improving oxygen delivery to tissues.
- Premature Newborn Anemia:
- EPO Production: In newborns, particularly premature ones, the liver produces most of the EPO. The liver's response to hypoxia is less sensitive than the kidneys', leading to a weaker production of EPO.
- Fetal Hemoglobin Transition: Fetal hemoglobin, which carries more oxygen, is replaced by adult hemoglobin after birth. Insufficient EPO production exacerbates anemia in newborns.
White Blood Cells
Types of White Blood Cells
White blood cells (WBCs), or leukocytes (LOO-ko-sites; "leuko-" meaning white), differ from red blood cells in that they have nuclei and do not contain hemoglobin. WBCs are classified into two main categories: granular and agranular, based on the presence or absence of conspicuous cytoplasmic granules visible under a light microscope after staining.
- Granular Leukocytes: These include neutrophils, eosinophils, and basophils.
- Neutrophils have small, evenly distributed, pale lilac granules and nuclei with two to five lobes connected by thin chromatin strands.
- Eosinophils contain large, uniform-sized granules that stain red-orange with acidic dyes, and their nuclei typically have two lobes connected by chromatin.
- Basophils have variable-sized granules that stain blue-purple with basic dyes, often obscuring the nucleus, which also has two lobes.
- Agranular Leukocytes: These include lymphocytes and monocytes. Although they possess cytoplasmic granules, these are not visible under a light microscope.
- Lymphocytes have a round or slightly indented nucleus that stains darkly, with cytoplasm forming a sky-blue rim around the nucleus. They vary in size from small (6-9 µm) to large (10-14 µm).
- Monocytes are larger (12-20 µm), with kidney-shaped or horseshoe-shaped nuclei and blue-gray, foamy cytoplasm. They differentiate into macrophages when they migrate into tissues.
Functions of White Blood Cells
WBCs play crucial roles in the immune system and have various lifespans, ranging from a few hours to several months or years, depending on the type and the presence of infections. Normal WBC counts range from 5,000 to 10,000 cells per microliter of blood.
- Leukocytosis: An increase in WBC count above 10,000/µL, typically a protective response to stressors such as infection, exercise, anesthesia, and surgery.
- Leukopenia: A decrease in WBC count below 5,000/µL, which is harmful and can result from radiation, shock, or certain chemotherapy agents.
Emigration and Phagocytosis
WBCs can leave the bloodstream through a process called emigration, formerly known as diapedesis, where they roll along the endothelium, stick to it, and squeeze through endothelial cells to reach sites of infection or inflammation. Adhesion molecules on endothelial cells and WBCs facilitate this process.
- Neutrophils and Macrophages:
Active in phagocytosis, these cells ingest bacteria and dispose of dead matter. Neutrophils respond quickly to bacterial infection, releasing chemicals like lysozyme and oxidants to destroy pathogens.
- Chemotaxis:
The movement of WBCs towards the site of infection is stimulated by chemicals released by microbes and damaged tissues.
Specific Types of White Blood Cells and Their Roles
Neutrophils
Neutrophils are the most abundant type of WBCs, constituting about 60-70% of all leukocytes. They are the body's first line of defense against infections, especially bacterial infections.
- Role in Infection: Neutrophils respond rapidly to the site of infection by moving out of the bloodstream and into the affected tissues. This process is known as chemotaxis, where they are attracted by chemical signals from the infection site.
- Phagocytosis: Once at the infection site, neutrophils engulf and digest pathogens through a process called phagocytosis. They contain granules filled with enzymes such as lysozyme and myeloperoxidase, which kill and digest the engulfed microorganisms.
- Oxidative Burst: Neutrophils produce reactive oxygen species (ROS) like superoxide anions and hydrogen peroxide, which are potent antimicrobial agents that help in destroying pathogens.
- Defensins: These proteins in neutrophils can puncture the cell membranes of bacteria, leading to their death.
Eosinophils
Eosinophils make up about 2-4% of the WBC population and are primarily involved in combating parasitic infections and participating in allergic reactions.
- Parasitic Infections: Eosinophils are particularly effective against multicellular parasites, such as helminths (worms). They release toxic proteins and free radicals that can kill parasites.
- Allergic Reactions: In allergic responses, eosinophils release enzymes like histaminase, which degrades histamine and helps modulate the inflammatory response. They also phagocytize antigen-antibody complexes, reducing the severity of allergic reactions.
- Chronic Inflammation: Eosinophils can contribute to chronic inflammatory conditions, such as asthma, by releasing mediators that sustain the inflammatory response.
Basophils
Basophils are the least common type of WBCs, making up less than 1% of the leukocyte population. They play a crucial role in allergic reactions and inflammation.
- Histamine Release: Basophils contain granules rich in histamine, heparin, and serotonin. When activated, they release these substances, causing vasodilation, increased permeability of blood vessels, and the recruitment of other inflammatory cells to the site of injury or infection.
- Allergic Reactions: Basophils are key players in the body's allergic response, contributing to symptoms such as swelling, redness, and itching.
- Interaction with IgE: Basophils have receptors for immunoglobulin E (IgE). Upon binding to IgE, they release their granule contents, which can intensify the inflammatory response.
Lymphocytes
Lymphocytes are critical components of the adaptive immune system and make up about 20-25% of the WBC count. They include three main types: B cells, T cells, and natural killer (NK) cells.
- B Cells: B cells are responsible for producing antibodies. When they encounter antigens, they differentiate into plasma cells, which secrete large quantities of antibodies specific to the antigen. These antibodies neutralize pathogens and mark them for destruction by other immune cells.
- T Cells: T cells have various roles in the immune response:
- Helper T Cells (CD4+ T cells): These cells coordinate the immune response by secreting cytokines that stimulate other immune cells.
- Cytotoxic T Cells (CD8+ T cells): These cells directly kill infected cells, cancer cells, and transplanted cells by inducing apoptosis (programmed cell death).
- Regulatory T Cells: These cells help maintain immune tolerance and prevent autoimmune responses.
- Natural Killer (NK) Cells: NK cells are part of the innate immune system and can destroy virus-infected cells and tumor cells without prior sensitization. They release cytotoxic granules that induce apoptosis in the target cells.
Monocytes
Monocytes account for about 3-8% of the WBC count and are the largest type of leukocytes. They play a significant role in the immune system's defense mechanisms.
- Phagocytosis: Monocytes are highly phagocytic cells that engulf and digest pathogens, cellular debris, and dead cells.
- Differentiation into Macrophages: Once they migrate into tissues, monocytes differentiate into macrophages. These can be either:
- Fixed Macrophages: Residing in specific tissues such as the liver (Kupffer cells), lungs (alveolar macrophages), and spleen.
- Wandering Macrophages: Moving throughout tissues to sites of infection or injury.
- Antigen Presentation: Macrophages process and present antigens on their surface to T cells, facilitating the adaptive immune response.
- Inflammation and Tissue Repair: Macrophages secrete cytokines and growth factors that promote inflammation and tissue repair, aiding in the healing process after infection or injury.
Platelets
Formation and Characteristics
Platelets, also known as thrombocytes, are small, disc-shaped cell fragments that play a crucial role in blood clotting and hemostasis.
-Development:
- Hemopoietic Stem Cells: Platelets originate from hemopoietic stem cells in the bone marrow.
- Thrombopoietin: Under the influence of the hormone thrombopoietin, myeloid stem cells develop into megakaryocyte-colony-forming cells.
- Megakaryoblasts: These cells then develop into precursor cells called megakaryoblasts.
- Megakaryocytes: Megakaryoblasts transform into megakaryocytes, which are large cells in the bone marrow.
- Fragmentation: Megakaryocytes splinter into 2000 to 3000 fragments. Each fragment, enclosed by a piece of the plasma membrane, becomes a platelet.
Structure:
- Size: Platelets are disc-shaped and measure 2–4 µm in diameter.
- Components: They contain many vesicles but lack a nucleus.
Functions
- Hemostasis: Platelets are essential in stopping blood loss from damaged blood vessels. When a vessel is injured, platelets adhere to the site, aggregate with each other, and form a temporary plug to seal the break
- Blood Clotting: Platelet granules contain chemicals that promote blood clotting. These chemicals are released upon platelet activation and contribute to the formation of a stable blood clot.
- Granules: Platelet granules release several substances that aid in the clotting process, such as adenosine diphosphate (ADP), thromboxane A2, and calcium ions.
- Clot Formation: These substances enhance the aggregation of platelets and the conversion of fibrinogen to fibrin, which stabilizes the clot.
- Lifespan and Removal:
- Lifespan: Platelets have a short life span, typically 5 to 9 days.
- Removal: Aged and dead platelets are removed from circulation by fixed macrophages in the spleen and liver.
BLOOD
✦✦✦✦✦✦✦✦✦✦✦